Safe Antidepressant Tapering Guide for Adults
Approximately 50% of adults experience withdrawal symptoms when discontinuing antidepressants too abruptly. This statistic underscores the critical need for a well-structured tapering process that minimizes these risks.
Understanding the various tapering methods and the importance of psychological support can greatly improve your experience. As you explore this topic further, you'll discover strategies that not only ease the change but also enhance your overall mental health outcomes.
From community resources, such as survivingantidepressants.org, an often safe guideline recommended is to reduce 10% each month. This is similar to "hyperbolic tapering", a method for gradually reducing the dosage of medications like antidepressants, where the size of the dose reductions becomes progressively smaller as the total dose decreases.
Understanding the Importance of Gradual Tapering
Understanding the importance of gradual tapering is essential, as abrupt cessation of antidepressant medication can lead to significant risks, including increased relapse rates and withdrawal symptoms.
Research shows that about 75% of individuals with recurrent depression experience relapse without ongoing treatment. A network meta-analysis found that slow tapering, lasting more than four weeks and combined with support, prevents relapses nearly as effectively as continuing standard-dose antidepressants.
Gradual tapering reduces both the frequency and severity of withdrawal symptoms compared to rapid reductions.
Clinical guidelines advocate for slow tapering, emphasizing the need for individualized plans based on factors like drug half-life and prior relapse history. This approach is particularly important because individualized tapering plans are essential for effective deprescribing.
The Role of Psychological Support During Tapering
As you navigate the tapering process, incorporating psychological support can greatly enhance your chances of a successful shift off antidepressants.
Research shows that adjunct psychological care, such as cognitive behavioral therapy (CBT) or mindfulness-based cognitive therapy (MBCT), considerably reduces relapse risks compared to tapering alone.
For instance, CBT can help improve coping skills and mood management, yielding relapse rates of 15-25% versus 35-80% with standard tapering methods. Additionally, studies indicate that 40-95% of individuals successfully discontinue antidepressants when psychological support is integrated into their tapering plan.
Regular treatment reviews and collaborative planning also enhance tapering outcomes, ensuring that you maintain stability while moving off medication. As a result, psychological support serves as an essential component of a safe tapering strategy, especially since slow tapering with psychological support has been shown to be as effective as continued medication for preventing relapse.
Recommended Tapering Speeds and Methods
A gradual and well-planned tapering approach is vital for those looking to discontinue antidepressant medication safely. Research indicates that slow tapering over more than four weeks greatly reduces the risk of relapse compared to abrupt discontinuation.
This method, especially when coupled with psychological support, can match the efficacy of continued standard-dose medication in preventing relapse. Tapering and discontinuing antidepressants is crucial for managing depression effectively.
Longer tapering periods yield higher success rates, while fast tapering often leads to increased relapse rates and lower discontinuation success.
It’s advisable to utilize appropriate formulations, such as liquid medications, to facilitate a slow taper. Ultimately, a careful balance between tapering rate and individual patient experience is essential for effective discontinuation.
Hyperbolic Tapering Techniques Explained
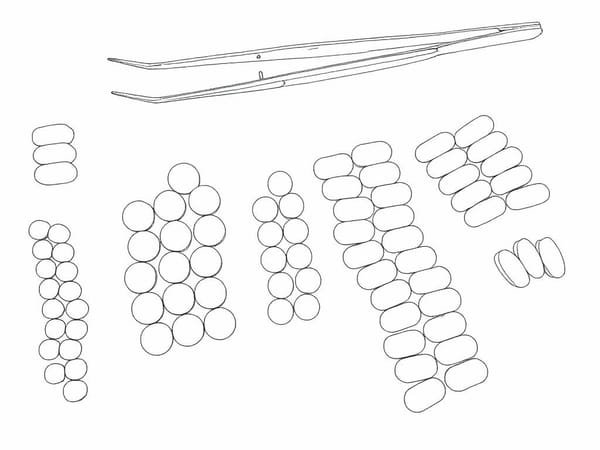
Hyperbolic tapering techniques represent a sophisticated approach to discontinuing antidepressant medications, characterized by dose reductions that decrease progressively in size as the dosage declines.
This method aims for a linear reduction in receptor occupancy rather than a simple milligram decrease, aligning pharmacologic changes with brain adaptation.
The Horowitz–Taylor model highlights that the final 10–15% of the dosage often requires extended tapering due to steep receptor occupancy at low doses. Evidence suggests that daily “tiny-step” reductions minimize withdrawal symptoms more effectively than weekly larger cuts.
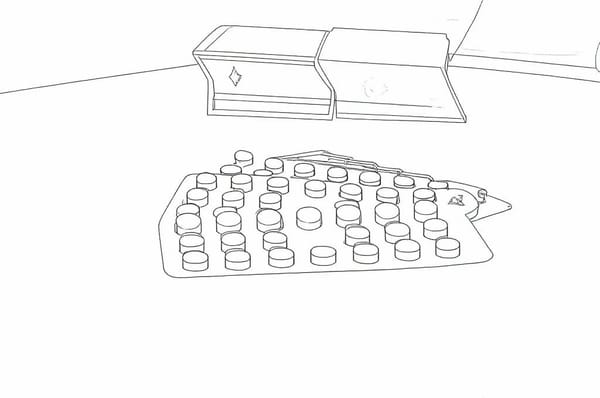
Implementing hyperbolic tapering may involve non-standard dose forms or tapering strips, allowing for precise adjustments based on symptom monitoring. This technique improves tolerability and adherence, making it a valuable strategy in antidepressant discontinuation, particularly as withdrawal symptoms are inversely related to taper rate.
Strategies for Switching Antidepressants Safely
When switching antidepressants, it’s essential to take into account various strategies that prioritize safety and efficacy. Selecting the appropriate strategy depends on the drug classes involved, half-lives, and the risk of interactions.
Common approaches include direct switch, cross-taper, taper plus immediate switch, and taper plus washout. A direct switch is typically reserved for similar classes, while cross-tapering is often preferred for different classes to maintain symptom coverage.
The taper, washout, and switch method minimizes interaction risks and is suitable for high-risk changes. Always consider the half-lives of the medications, especially with long-acting agents like fluoxetine, which require extended washout periods.
Choosing a strategy that balances the risk of relapse and withdrawal symptoms effectively is crucial for monitoring during and after switching.
Managing Withdrawal Symptoms Effectively
Managing withdrawal symptoms effectively requires a thoughtful approach, especially since abrupt discontinuation of antidepressants can lead to considerable discomfort.
You may experience flu-like symptoms, nausea, and heightened anxiety, especially if you’ve used SSRIs or SNRIs for an extended period. Gradual tapering markedly reduces these risks, making it essential to avoid sudden cessation.
Consider pharmacological interventions like switching to a longer half-life antidepressant or using liquid formulations for precise dosing.
Lifestyle measures such as regular exercise, hydration, and a balanced diet play an important role in your adjustment. Keeping a mood diary can help track your symptoms, while therapy offers support and coping strategies.
Always consult your healthcare provider to monitor your progress and adjust your plan as needed. Gradual tapering is recommended to minimize withdrawal symptoms and ensure a smoother transition.
Monitoring Progress and Adjusting the Tapering Plan
While managing the tapering process of antidepressants, it’s vital to monitor your progress closely and adjust your tapering plan as needed.
Monitoring your progress during antidepressant tapering is essential for safe and effective adjustments to your plan.
Regular clinical monitoring through frequent appointments allows your provider to assess your symptoms and make necessary adjustments to your tapering schedule.
You should also engage in patient self-tracking by logging daily mood, sleep patterns, and physical changes, which can inform your provider about your experiences. Tapering is recognized as a crucial process for safely discontinuing antidepressant medication, aiming to minimize potential withdrawal symptoms.
Individualized adjustments are important, as the tapering approach must reflect your unique history and response. Utilize objective progress indicators, such as dose reduction milestones and mental health stability, to gauge success.
Finally, maintaining flexibility in your plan guarantees safe and effective adjustments based on ongoing evaluations and shared decision-making.