Safe Cross Tapering Of Antidepressants Explained
When I switched from one antidepressant to another, it felt like walking a tightrope—one misstep could send me tumbling into a dark place. Safe cross-tapering is more than just swapping meds; it’s a delicate dance of reducing the old medication while carefully introducing the new one.
You need to stay alert for any mood shifts or side effects, and having open lines of communication with your doctor is essential. What happens if you don't?
Key Takeaways
- Cross-tapering involves gradually reducing the first antidepressant while introducing a second to maintain treatment and minimize withdrawal symptoms.
- A typical cross-tapering process spans 2 to 4 weeks, monitored closely for mood changes and side effects.
- Consult a healthcare provider to create a personalized tapering schedule based on medication history and individual responses.
- Be vigilant for signs of serotonin syndrome when switching medications, especially with SSRIs, SNRIs, or MAOIs, and seek immediate help if severe symptoms occur.
- Open communication with your doctor throughout the process is crucial for adjusting the plan and ensuring patient safety and well-being.
What Is Cross-Tapering and Why Is It Important?
When you’re maneuvering the tricky waters of switching antidepressants, cross-tapering can feel like the lifeline you didn’t know you needed.
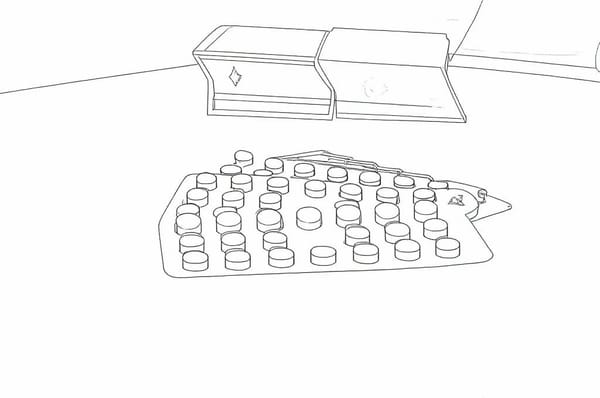
This method involves gradually lowering the dose of your first antidepressant while gently introducing a second at a low dose, allowing you to navigate through the change without an abrupt stop.
You’ll be taking both medications for a brief overlap, which helps maintain therapeutic coverage and minimizes withdrawal symptoms. The process usually spans 1-2 weeks, tailored to your unique needs.
It’s important to note that tapering is recommended to minimize the risk of antidepressant discontinuation syndrome, which can affect up to 20% of people who use antidepressants. Close monitoring is essential during this time, helping catch any adverse effects or changes in your mood. It’s a safer, smoother shift that supports your mental well-being, ensuring you don’t have to face the storm of switching alone.
Benefits of Cross-Tapering Compared to Other Switching Methods
Cross-tapering isn’t just a strategy; it’s often a lifeline during the challenging task of switching antidepressants.
Think of it as a safety net that keeps you from falling into the abyss of depressive symptoms when you’re shifting from one medication to another. By overlapping medications, you maintain a steady flow of treatment, which helps manage those pesky withdrawal symptoms and reduces the risk of relapse.
Studies show you can still experience symptom improvements during this change, making it feel less like a rollercoaster ride. It’s also safer—consider it a gentle bridge between two worlds, minimizing the risk of adverse effects.
In a way, cross-tapering offers you a personalized route, giving you and your clinician control over your mental health journey. The increase in mental health care needs has made cross-tapering an essential practice for primary care providers managing complex medication transitions.
How to Begin Cross-Tapering Your Antidepressants
Starting the journey of cross-tapering your antidepressants can feel a bit like standing at the edge of a cliff, peering into the unknown, but with the right approach, you can navigate this shift with confidence.
First, assess your current medication's history, noting the dose, duration, and any side effects you've faced. Your doctor will help determine a tapering schedule, often stretching over one to two weeks. It’s important to remember that during this process, noticeable improvements typically take 1 to 3 weeks after you start the new medication.
As you gradually reduce your first antidepressant, they'll introduce the new one at a low dose, cautiously increasing based on your response. Keep a close eye on withdrawal symptoms like headaches or irritability, and don’t hesitate to speak up if things feel off.
Recommended Timeline for Cross-Tapering Antidepressants
Steering the timeline for cross-tapering antidepressants can feel like charting a course through uncharted waters, where each wave of emotion may catch you off guard.
Typically, you’ll want to allow 2 to 4 weeks for the cross-taper, but it can stretch longer if you’ve been on medication for months or years. It's essential to remember that cross-tapering is generally recommended for most antidepressants, typically taking 2 to 4 weeks for the transition.
Allow 2 to 4 weeks for cross-tapering, but expect it to take longer if you've been on medication for an extended period.
If you’re switching from one antidepressant to another, know that your pace will depend on how your body responds. Start with gradual reductions and keep a close eye on your symptoms.
If withdrawal hits hard, slow down and consider returning to your previous dose. Each switch requires careful navigation, so be open with your healthcare provider and adapt your plan as needed.
Trust and stick to the process, even when it feels rocky.
Antidepressants That Can Be Safely Cross-Tapered
When you're contemplating the delicate dance of switching between antidepressants, it’s essential to understand which medications can be safely cross-tapered.
Here’s a quick guide to help you navigate this tricky change:
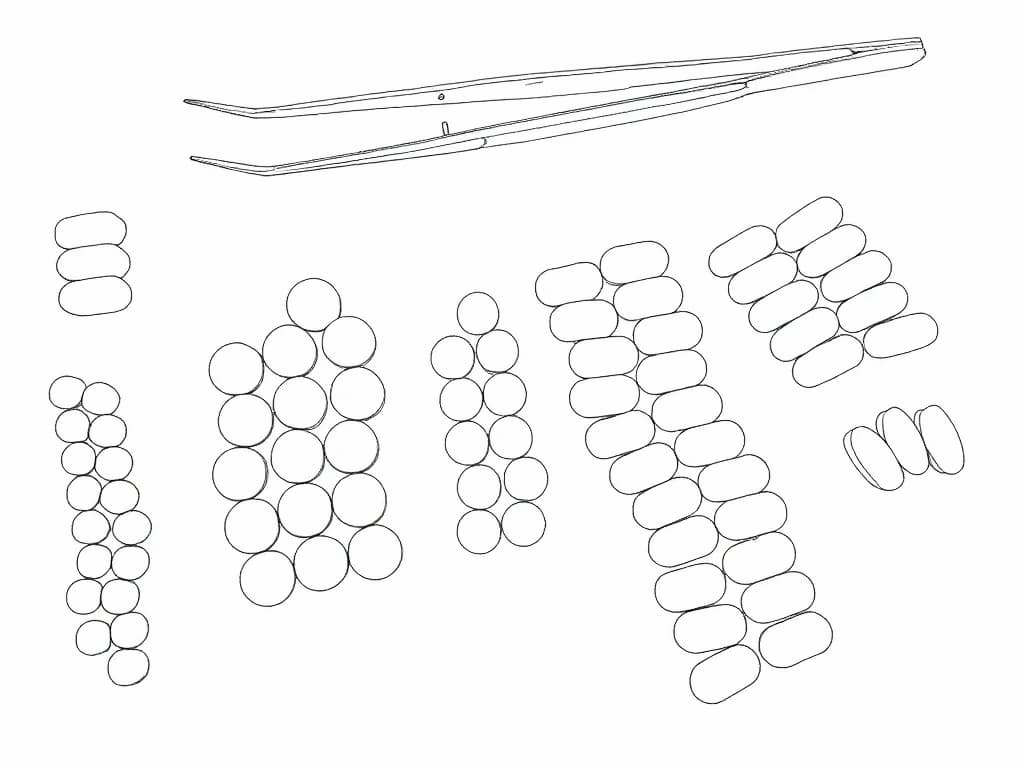
- SSRIs to Other Antidepressants: High-dose SSRIs require cross tapering, while low-dose switches to venlafaxine or duloxetine can be direct. In cases where two SSRI trials fail, consulting the BHI team is crucial.
- SNRIs to Other Antidepressants: Cross tapering is advised, but low doses of duloxetine or venlafaxine allow for direct switches.
- Bupropion Switches: Generally recommended to cross taper due to minimal serotonergic effects.
- Mirtazapine Switches: Always use the cross taper method to reduce risks of discontinuation.
Understanding these options can ease your journey and help you find a stable footing on the path to better mental health.
How to Monitor Side Effects While Cross-Tapering
As you initiate the complex journey of cross-tapering antidepressants, staying vigilant about potential side effects can feel like walking a tightrope—one misstep, and you might find yourself grappling with uncomfortable symptoms or even a significant emotional downturn.
To navigate this delicate process, review your progress within two weeks of starting the new medication, and monitor weekly for mood changes and suicidal thoughts. Keep a close eye on common withdrawal symptoms like dizziness or irritability, and use the Discontinuation-Emergent Signs and Symptoms scale to track your experience.
It's also important to remember that up to 60% of patients show a response within the first two weeks of treatment, which may help you gauge the effectiveness of the new medication.
If you notice intolerable side effects, don’t hesitate to adjust your tapering pace. Education is essential; understanding what to expect can empower you to communicate openly with your healthcare provider, ensuring a safer shift.
What Are the Risks of Serotonin Syndrome?
While you might be focused on the benefits of your new antidepressant, it’s crucial to remember that the risks of serotonin syndrome can lurk in the shadows, ready to surprise you when you least expect it. This condition arises from too much serotonin and can range from mild discomfort to life-threatening scenarios.
Be cautious: the risks of serotonin syndrome can emerge unexpectedly, turning the benefits of your antidepressant into a serious concern.
Here are some critical points to take into account:
- Causes: A mix of serotonergic medications or supplements can trigger it.
- Symptoms: You might experience anything from tremors to confusion or even seizures.
- Risk Factors: Starting a new medication or increasing your dose can heighten your chances, especially when multiple drugs that affect serotonin levels are involved.
- Outcomes: While mild cases may resolve on their own, severe ones can lead to organ failure if untreated.
Stay vigilant!
When to Consult a Specialist for High-Risk Switches?
Maneuvering the world of antidepressants can feel like walking a tightrope; one misstep could lead to a serious fall.
If you’re considering high-risk switches—like moving from SSRIs to SNRIs or shifting to MAOIs—don’t go it alone. A specialist can help navigate potential withdrawal symptoms or worsening mood.
If you’ve had past issues with discontinuation syndrome, or if you’re dealing with severe symptoms or suicidal thoughts, it’s essential to seek expert advice. You shouldn’t ignore intolerable side effects or drug interactions, either; they’re like warning bells. High treatment failure rates necessitate knowledge of safe and effective switching strategies.
Regular monitoring and tailored strategies are critical for your safety. Remember, it’s not just about crossing over; it’s about staying balanced and secure on that tightrope.
Contraindications: What to Avoid During Cross-Tapering
When you’re in the thick of cross-tapering antidepressants, it’s essential to recognize what to steer clear of, especially since the stakes can feel alarmingly high.
Avoiding certain combinations and overlaps can save you from a whirlwind of complications. Here’s a quick list of what to watch out for:
- Never cross-taper SSRIs with clomipramine or moclobemide—the risk of serotonin syndrome is serious.
- Don't overlap MAOIs with SSRIs or SNRIs—it’s a hard no; you need a proper washout period.
- Skip fluvoxamine with agomelatine—the potential for increased side effects isn’t worth it.
- Steer clear of combining SSRIs with tricyclics—the toxicity risks can skyrocket. Pharmacodynamic interactions can occur when two antidepressants affect the same neurotransmitter system, leading to worsening side effects.
Stay vigilant, and remember that your well-being deserves careful attention during this process.
Cross-Tapering Tips for Success
Steering through the tricky waters of cross-tapering antidepressants can feel a bit like walking a tightrope—one misstep and you might find yourself in a world of discomfort.
To keep your balance, start by gradually reducing your first antidepressant, aiming for around 25% less each week, taking it slow if you’ve been on it for a while.
Introduce the new medication at a low dose, increasing it as you decrease the old one. It's important to remember that approximately two-thirds of patients with major depression do not respond adequately to the first prescribed medication, highlighting the necessity of careful management during this transition.
Monitor your symptoms closely during this shift; schedule monthly check-ins to assess how you’re doing.
Remember, it’s essential to communicate openly with your doctor about how you’re feeling.
If things get rough, it’s okay to pause and reassess—your well-being is the priority.