Amitriptyline Tapering Guide for Safe Withdrawal
Maneuvering the intricate landscape of amitriptyline withdrawal can feel like walking a tightrope, where balance is vital to avoid a fall into discomfort or distress.
Tapering off this medication requires a careful approach to minimize withdrawal symptoms and prevent rebound depression.
Understanding the reasons for tapering and the strategies involved is essential for a successful changeover. So, what are the best practices to guarantee a safe and effective withdrawal process?
Understanding Amitriptyline and Its Uses
Amitriptyline, a tricyclic antidepressant (TCA), plays a significant role in the management of various mental health and pain-related conditions. It primarily increases serotonin and norepinephrine levels in the brain, enhancing mood and emotional balance.
It is also effective in managing chronic pain conditions, making it a versatile option for patients with overlapping health issues.
You’ll find it effective for major depressive disorder, especially in cases of endogenous depression. Beyond treating depression, amitriptyline is useful in managing neuropathic pain, migraines, and chronic tension-type headaches. Its analgesic properties can also alleviate conditions such as fibromyalgia and diabetic neuropathy. It exhibits anticholinergic and sedative effects, making it suitable for certain individuals experiencing insomnia.
Understanding these uses can help you and your healthcare provider determine if amitriptyline is the right choice for your treatment needs.
Why Tapering Is Essential
Tapering off amitriptyline is a crucial process for anyone considering discontinuation of this medication. Abrupt cessation can lead to antidepressant discontinuation syndrome (ADS), which includes uncomfortable flu-like symptoms and sensory disturbances.
Tapering is essential to minimize these risks. A gradual reduction helps prevent rebound effects, such as the return of depression or insomnia. This process allows your body to adjust to changes in serotonin and norepinephrine levels, promoting a smoother change.
Careful tapering enhances safety by monitoring potential medical risks, including cardiac issues and dehydration. By following a structured tapering plan, you can optimize your comfort during withdrawal and guarantee a more manageable experience overall.
It’s important to remember that physical dependence can occur with amitriptyline, emphasizing the need for a careful, slow and gentle approach to discontinuation.
Common Withdrawal Symptoms
Discontinuing amitriptyline can lead to a range of withdrawal symptoms that may greatly impact your daily life.
Physically, you might experience nausea, sometimes accompanied by vomiting and diarrhea, alongside stomach cramps. Neurologically, dizziness and heightened headaches are common, often peaking during the first week. You may also encounter sensory disturbances, such as burning sensations or brain zaps.
Flu-like symptoms, including fatigue, muscle aches, and chills, can mimic illness. Sleep disturbances, like insomnia and vivid dreams, may disrupt your rest, contributing to feelings of lethargy. It is important to note that these withdrawal symptoms may affect a significant percentage of individuals who discontinue the medication suddenly.
Psychologically speaking, heightened anxiety, irritability, and mood swings can emerge, affecting your overall well-being. Recognizing these symptoms is essential for steering your tapering journey effectively.
Evidence-Based Tapering Strategies
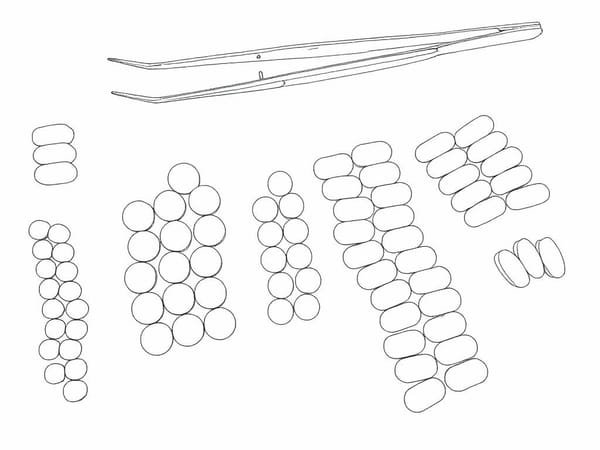
When considering a reduction in amitriptyline dosage, evidence-based tapering strategies play an indispensable role in minimizing withdrawal symptoms and ensuring a smoother shift.
Hyperbolic tapering, which involves proportional dose reductions, can help reduce significant pharmacologic shifts, particularly at lower doses.
In contrast, linear tapers can lead to larger changes in receptor occupancy, increasing withdrawal risks. Clinical guidelines advocate for slow tapering over weeks to months, recommending reductions of 10–25% per step with intervals of 3–7 days up to 4-weeks. Individualization of the tapering strategy is vital, considering factors like duration of use, current dosage, and patient history.
For some, micro-tapering may be necessary, ensuring that the final reductions are minimal to further ease discontinuation effects. Gradual tapering is essential to reduce the risk of withdrawal symptoms, particularly for patients with a history of long-term medication use.
Clinical Management and Monitoring
Effective clinical management and monitoring during the tapering of amitriptyline are fundamental for ensuring patient safety and minimizing withdrawal symptoms.
Close supervision by your prescribing clinician allows for timely assessment of your responses at specified intervals. If withdrawal symptoms emerge, adjustments to the tapering pace, such as pausing or slowing reductions, may be necessary.
Common symptoms, including mood changes and gastrointestinal disturbances, often arise within the first week and can persist for weeks to months. Recognizing these symptoms is essential; report any troubling experiences to your provider. Monitoring parameters like hydration, blood pressure, and potential cardiac issues is critical.
Implementing supportive strategies, including stress management and healthy habits, can further facilitate a smoother tapering process. Tapering and discontinuing antidepressants is crucial for managing depression effectively.
Individual Factors Influencing Tapering Speed
Several individual factors considerably influence the speed at which you can safely taper amitriptyline. Your duration and dose of use play vital roles; long-term users or those on higher doses often require slower tapers to mitigate withdrawal symptoms.
Your metabolic profile, particularly with CYP2D6 and CYP2C19 enzymes, affects how quickly your body processes the medication. If you've experienced difficult withdrawals in the past or if you're taking other medications that interact with amitriptyline, these factors necessitate a more cautious approach.
Your overall clinical profile, including any comorbid conditions, can further shape your tapering strategy, making it essential to tailor the process to your unique circumstances for the safest experience possible. Amitriptyline's mechanism of action involves blocking the reuptake of serotonin and norepinephrine, which can impact your withdrawal experience depending on individual neurochemistry.
Non-Drug Supports During Withdrawal
Non-drug supports during withdrawal from amitriptyline play an essential role in facilitating a smoother change and enhancing overall well-being.
A balanced diet, rich in protein, complex carbohydrates, and healthy fats, supports neurotransmitter synthesis, helping to stabilize mood. Regular, low-glycemic meals maintain stable blood sugar levels, reducing irritability and fatigue.
Managing neurotransmitter imbalances during this time can also contribute to overall emotional stability.
Staying hydrated is vital, aiming for clear or light-yellow urine to support circulation and energy. Limiting caffeine and alcohol can diminish sleep disruption and anxiety.
Establishing good sleep hygiene, including a regular sleep-wake schedule and a calming pre-sleep routine, can greatly improve sleep quality.
Incorporating moderate physical activity, such as walking or yoga, promotes relaxation and mood enhancement, further aiding in the withdrawal process.
Safety Precautions to Consider
During the withdrawal process from amitriptyline, it’s essential to prioritize safety precautions to mitigate potential risks associated with discontinuation.
Avoid abruptly stopping the medication, as this can lead to severe withdrawal symptoms, including dizziness, headaches, and gastrointestinal upset. Gradual tapering is vital; consider reducing your dose by 10% every 1–2 weeks, adjusting based on your symptoms. Gradual tapering is crucial to minimize withdrawal symptoms.
Monitor your physical safety, especially regarding balance and alertness, as dizziness and fatigue may impair your ability to perform tasks safely. Maintain hydration and nutrition to support stability during withdrawal.
Finally, keep track of your symptoms closely, as early observation can facilitate timely adjustments to your tapering strategy, ensuring a safer and more manageable withdrawal experience.
When to Seek Medical Assistance
Recognizing when to seek medical assistance during the amitriptyline tapering process is essential for ensuring your safety and well-being.
If you experience new or worsening depression, especially after reducing your dose, it’s vital to consult a healthcare professional. Suicidal thoughts or behaviors during this time constitute a medical emergency, requiring immediate help.
Severe anxiety, panic attacks, or agitation that disrupts daily life necessitates urgent assessment. Security measures are in place on certain websites to protect users, and understanding this can help you remain calm if you encounter access issues.
Watch for physical symptoms like extreme dizziness or irregular heartbeat, which could indicate serious complications.
If withdrawal symptoms persist for weeks without improvement or escalate in severity, reach out to your clinician.
Timely intervention can prevent serious consequences and support a safer tapering experience.
Long-Term Considerations After Tapering
As you complete the tapering process of amitriptyline, it's important to reflect on the long-term implications for your mental health and overall well-being.
While many individuals experience favorable outcomes, the risk of symptom recurrence remains significant, with studies indicating that up to 80% may relapse into depression within weeks.
This high risk of depression recurrence underscores the importance of closely monitoring your mood, sleep patterns, and daily functioning over the following months, as lingering issues could suggest a return to the original condition rather than mere withdrawal.
Consider non-drug strategies like sleep hygiene and relaxation training to manage persistent symptoms.
If you encounter significant challenges, reassessing your treatment plan with a healthcare professional can provide necessary support and guidance for steering this change successfully.